What was RIO NHS
In 2008, based on estimates from local data, an estimated 60% of the local Rotherham population was overweight or obese, in line with the national average (although 22% had no recorded Body Mass Index, or BMI). The National Child Measurement Programme (NCMP) data for showed that our childhood prevalence rates for those overweight or obese, were similar, but slightly higher than the national average.
NHS Rotherham agreed to make £3.5m available to fund their NHS obesity strategy for a 3 year pilot period. The Rotherham Obesity Strategy Group (ROSG) was then given the responsibility of finalising detailed service specifications for each tier of intervention, and the public health lead for obesity, Carol Weir, was given responsibility as lead commissioner. NHS Rotherham’s Healthy Weight Commissioning Framework proceeded to win the 2009 NHS Health and Social Care Award.
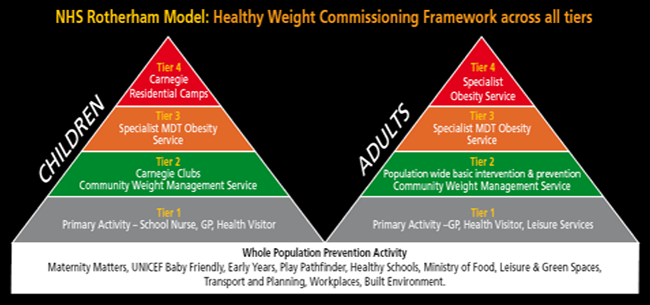
The Rotherham Obesity Strategy for the management of healthy weight in adults and children involves 4 tiers of intervention.
Below is a diagram outlining the Framework as it was in 2009.
The initial level of intervention is the primary activity most often done in the primary care setting, which involves identifying those patients that have weight problems and are motivated to change, especially those with, or at risk from, serious medical co-morbidities. It is important to clarify that this primary activity, and any associated health promotion advice, could, and still can be delivered by any healthcare professional from primary or secondary care, or in the pharmacy, council, leisure services, or private sector.
The 2nd tier of intervention is a community based, time limited, weight management programme of diet, nutrition, lifestyle and exercise advice delivered by trained staff.
For adults, between 2009-14, this was delivered by the Reshape Rotherham programme overseen by the local dietetics department, and for children this is the More Life (formerly Carnegie) Clubs programme delivered by Places for People leisure (formerly DC Leisure). Patients can self-refer to these services, or be referred by an appropriate healthcare professional after an assessment of motivation. From 2014, the adult tier 2 service was delivered by Shape Up, and the child service continued to be delivered by Places for People Leisure using the More Life model.
Those patients who did not meet their healthy weight targets in this 2nd level of intervention, or for those who are considered to be more at risk of the cardiometabolic consequences associated with obesity (such as diabetes and cardiovascular disease) and required more specialist intervention, were referred into the tier 3 intervention, which is a specialist centre for weight management. This service is delivered by the Rotherham Institute for Obesity (RIO).
After 2014 the integrated framework of services was referred to as Weigh Up Rotherham, and it had a Single Point of Access (although this was in addition to direct referrals to service providers, and relying on self-reported weights and medical problems).
The NHS Healthy Weight Framework was decommissioned from 12 July 2017.
Summary of job description and role at NHS RIO
The RIO Multidisciplinary Team Approach
The Rotherham Institute for Obesity (RIO) was a specialist centre for the management of weight problems with a multidisciplinary approach to reducing and maintaining weight loss. RIO did not claim to have invented the cure for weight problems, and could not guarantee weight loss for patients, but it brought together all the NHS approved and evidence-based methods for weight loss into one Primary care based Centre in the hope that they could maximise the chances for weight loss. The RIO multidisciplinary team (MDT) was made up of a number of specialist individuals, who all have distinct roles, but worked together for the benefit of the patient, with regular MDT meetings to discuss individualised patient care. The team worked in a specially designed centre, with specialist facilities and resources, but with the same ease of access normally associated with the primary care setting.
It was intended that the majority of patients that required the services provided by RIO would be those who have received the initial tiers of weight management intervention offered locally but considered unsuccessful in their level of weight loss. Patients could also be referred directly to RIO via local general practitioners, or medical practitioners at the local hospital, if they meet specific criteria that deemed them to be particularly at risk of the cardio-metabolic consequences of obesity, such as diabetes, or need any of the more specialist intervention offered by RIO. Care pathways were developed to allow referrals for patients who may have accessed, yet been unsuccessful in, other accredited weight management programmes that may be offered locally by pharmacists or in the private sector.
When patient referrals were initially received they are triaged to assess which, if not all, of the services offered by RIO were required, and appointments made as appropriate. All patients were initially assessed in a dedicated weighing and measuring room and all parameters including blood pressure, weight, height, body mass index (BMI), and fat composition using bio-impedance scales, were taken. Regularly calibrated weigh-bridge scales are used in order to provide consistency of measurements for weights of morbidly obese levels, and for patients with limited mobility or wheelchair users. If no recent blood tests had been performed these are taken on-site in order to exclude previously undiagnosed metabolic conditions, such as diabetes and pre-diabetic states, thyroid disorders, dyslipidaemia (abnormal levels of cholesterol/fat), or non-alcoholic fatty liver disease (NAFLD).
Comprehensive dietetic advice was delivered by a number of specialists within the team, ranging from basic principles delivered by the Obesity Specialist Nurses (OSNs) and Healthcare Specialists, to nutritional and cooking skills advice delivered by the “Cook & Eat” team (in on-site kitchen facilities) and more detailed advice from the dietitian when needed and appropriate. RIO had a specialist RIO dietitian who would also deliver tailored advice to patients with more complex dietary needs, such as those with celiac disease, malabsorption syndrome, type 1 diabetes, IBS, vegan or South Asian diets, as well as those pre- and post- op bariatric surgery. The specialist RIO dietitian worked with other members of the team, such as the GP with Specialist Interest (GPwSI)/bariatric physician and the OSNs to initiate and support patients that were considered appropriate for Liquid Low Energy Diets (LLEDs) or Very Low Calorie Diets (VLCDs), or those patients involved in research studies.
All patients received further basic dietary and nutritional advice as well as lifestyle and exercise education throughout the length of time they were in the service. The RIO weight loss programme was normally 6 months, but had an open door policy for re-referral as it accepted that obesity is a chronic relapsing condition.
There were opportunities to discuss other aspects of their lives that may have been a barrier to successful weight loss, with Health Trainers, Talking Therapists proficient in techniques such as Cognitive Behavioural Therapy (CBT), Neuro Linguistic Programming (NLP), Emotional Freedom Techniques (EFT), and Hypnotherapy, or access to a Psychologist.
Appointments could be made with an Exercise Therapist, who could help to tailor a specific exercise programme suitable for the individual (provided in on-site gym facilities), and patients were then encouraged to engage with free and subsidised local leisure facilities that had been arranged through partnerships with RIO. Specialist equipment for both adults and children were used in our on-site gym, but they also engaged with techniques such as “exer-gaming” (Wii, Wii-Fit, X-box Kinect) which was now approved as being an effective tool for increasing physical activity.
Patients that were to be considered for weight loss pharmacotherapy, or that have screened positive for possible Obstructive Sleep Apnoea (OSA) were reviewed by the GPwSI. This was an opportunity to review current medications that may have been associated with weight gain, and recommendations made to change them to newer, more weight-friendly, alternatives. Weight loss pharmacotherapy such as Orlistat may have been prescribed, with all on-going prescribing of any weight loss pharmacotherapy done by RIO, with the support of local GPs and the medicines management team, in order to maintain consistent and safe prescribing according to strict protocols.
Obstructive Sleep Apnoea (OSA) is currently an under-diagnosed and potentially fatal condition that is more prevalent in the obese population, in particular obese patients with diabetes. RIO became the first centre anywhere in the UK to routinely screen these high-risk populations, not just with questionnaire based screening but also with overnight oximetry equipment. When screened as positive these patients are fast-tracked to the local sleep clinic. Original data published by RIO has shown that this is an accurate and effective technique with very high correlation to subsequent need for treatment at secondary care.
RIO was considered a specialist service and most patients come to RIO having tried tier 2 group interventions (community weight management programmes such as Reshape Rotherham or commercial organisations such as Weight Watchers or Slimming World) previously. Therefore, due to patient demand, the majority of their consultations were one-to-one in dedicated consulting rooms, although group work was available, and often works well for nutritional advice or talking therapies. Further facilities within the Institute included a dedicated meeting room which had been developed to allow educational meetings for patients or healthcare professionals. This room also provided a resource library with computer terminals, books and journals and many other educational tools. It was hoped that in the future the service will work with other centres to form part of further research into the management of obesity, diabetes and other related conditions.
RIO Success
Patients going through the RIO service were considered a success if they meet certain criteria depending on the individual. For example, for most patients this may be considered to be 3-5% weight loss at 3 months, maintained at 6 months, or minimum 5% weight loss at 6 months (for adults). For other patients it may have be more, however, in the case of certain children, weight maintenance alone may have been considered a successful goal. The use of bio-impedance has also demonstrated that in patients that do not initially appear to reach their weight loss targets, they had demonstrable improvements in other aspects, such as reduced body fat and increased lean muscle (published data at the European Congress of Obesity 2014) as well as improved well-being scores.
A summary of previously published data showed that for those patients who completed the 6m RIO weight loss programme, the annual success rate was:
- 96% of adults lose weight
- 71% of adults met or did better than Rotherham commissioned weight loss targets. With annual weight loss in adult responders of 5.1 tons, with average weight loss of 6.7 kgs (14.7 lbs)
- 50% reduction in the anticipated numbers requiring a referral for bariatric surgery
- 72% of children met or did better than Rotherham commissioned weight loss targets
The cumulative weight loss by July 2017 was a staggering 33.7 tons!
Engagement and satisfaction
RIO consistently received nearly 2000 referrals per year from primary and secondary care.
Locally published data showed that all 41 individual Rotherham GP Practices (or branch surgeries) regularly referred into the service. Similarly they received referrals from numerous departments within their local secondary care service, such as diabetologists, gynaecologists, rheumatologists, musculoskeletal service, as well as paediatrics.
They were very well liked and appreciated by their patients, and achieved a 97% patient satisfaction with the service (76% reported “excellent”) in patient satisfaction questionnaires.
Health savings from a “trip to RIO”
RIO also served an important role in the pre-op and post-op care for patients requiring referral for bariatric surgery. Prior to the NHS England policy document on bariatric surgery in April 2013, all NHS Rotherham patients meeting local specialist commissioning group criteria for NHS funding (BMI > 50 or BMI > 45 with co-morbidity) had to come through RIO services and be triaged on the appropriateness of the referral. Over the last few years before decommissioning, a RIO audit had shown that this has seen a reduction in inappropriate referrals to bariatric surgical centres, and an overall cessation of the year on year increase in referrals for surgery, due to the success that the MDT approach had on weight loss in the morbidly obese that would have otherwise required surgery. There had consistently been over a 50% reduction in bariatric surgery, compared with the anticipated numbers expected to be referred, which had been estimated to have saved more money that the overall adult tier 3 service costs to run. This had not been because RIO had introduced further barriers to patients, making it more difficult to access surgery, but because of successful medical management, eg, one of their patients made the front pages of the local newspapers for having lost an impressive 23 stones in weight without surgery!
As well as reducing the costs associated with expensive, and more invasive, interventions such as bariatric surgery, they noted that patients losing weight in RIO had a reduction in their prescribed medications. It was hoped that with this would be an associated reduction in their visits to see their local GPs and/or nurse clinics, a reduction in the amount of admissions to hospital for obesity related disease, and an indirect reduction in the number of patients on benefits due to weight related problems. These additional savings add to the health economic argument for actively treating obesity.
The overall Rotherham Healthy Weight Framework cost less than £1m per year for all activity in tiers 1 & 2, RIO for both adults and children, and tier 4 children (residential camps), ie, everything except the bariatric surgery. This was to provide gold standard services to a population of more than 260,000 patients. If this had been scaled up for the UK population (approximately 60 million patients) this would cost an estimated £240m. This might sound a lot in a recession, but it is still significantly less than he estimated direct and indirect costs of obesity projected for 2050 by the Foresight Report of 2007, which is £49.9bn per year. Instead the latest figures suggest that services like RIO are on the decline due to funding cuts.
RIO also served an important role in the triage of morbidly obese children who may have requested the attendance at the residential weight management camps. Suitable patients could have an assessment for underlying medical conditions, psychological issues, or any outstanding social or learning problems. As was the case of adult surgical triage, this process could increase the likelihood of more appropriate referrals to this more intensive and expensive resource. Furthermore, whilst any children were attending the More Life (formerly Carnegie) Residential Camps, RIO would provide support and educational advice to the families of these children, to reinforce knowledge and reduce the likelihood that the child returns to an obesogenic environment.
A fully integrated care pathway existed in both directions through the tiers of the overall obesity strategy, and patients would come back to RIO after any tier 4 intervention. All 4 tiers would liaise on a regular basis, either at regular all-provider meetings, or individually as necessary to discuss patient care. Results from the service are regularly audited and the overall Rotherham obesity strategy was subject to a regular monitoring process by service providers and members of Public Health.
RIO, in particular, was very keen on publishing its data, and this can be found in the public domain.











